Faeces collected using Blue Picker or Green Picker
For a limited period, FIT testing can be performed on a BLUE or GREEN top faecal picker device. We will only provide GREEN top devices for all new orders. Devices are expensive: we ask that you use up all current supplies of BLUE top devices first.
The Quantitative Faecal Immunochemical Test (qFIT) is a test to detect hidden or ‘occult’ blood in stool samples. Unlike older FOB tests, qFIT test uses antibodies that specifically recognise human haemoglobin and are consequently more sensitive and specific tests than the guaiac based FOB test. It also allows the amount of haemoglobin to be measured.
Faecal occult blood tests should be offered to adults without rectal bleeding who were classed as “low risk, but not no risk” of having colorectal cancer.
These are patients who are:
NICE DG30 guidance encourages use of the test for any patient with abdominal symptoms who doesn’t fit the NG12 2WW criteria.
FIT testing can also be requested for patients who are ≥18 years who have vague symptoms.
IMPORTANT UPDATE: From 19th March 2024 Royal Devon & Exeter and North Devon District Hospital facing practice should order FIT tests on ICE – For more information please follow this link
NEW ICE ordered collection instructions, please follow this link
Derriford and Torbay Hospital facing practices should follow the instructions below –
FIT packs will be delivered to each GP practice the packs have an outer envelope.
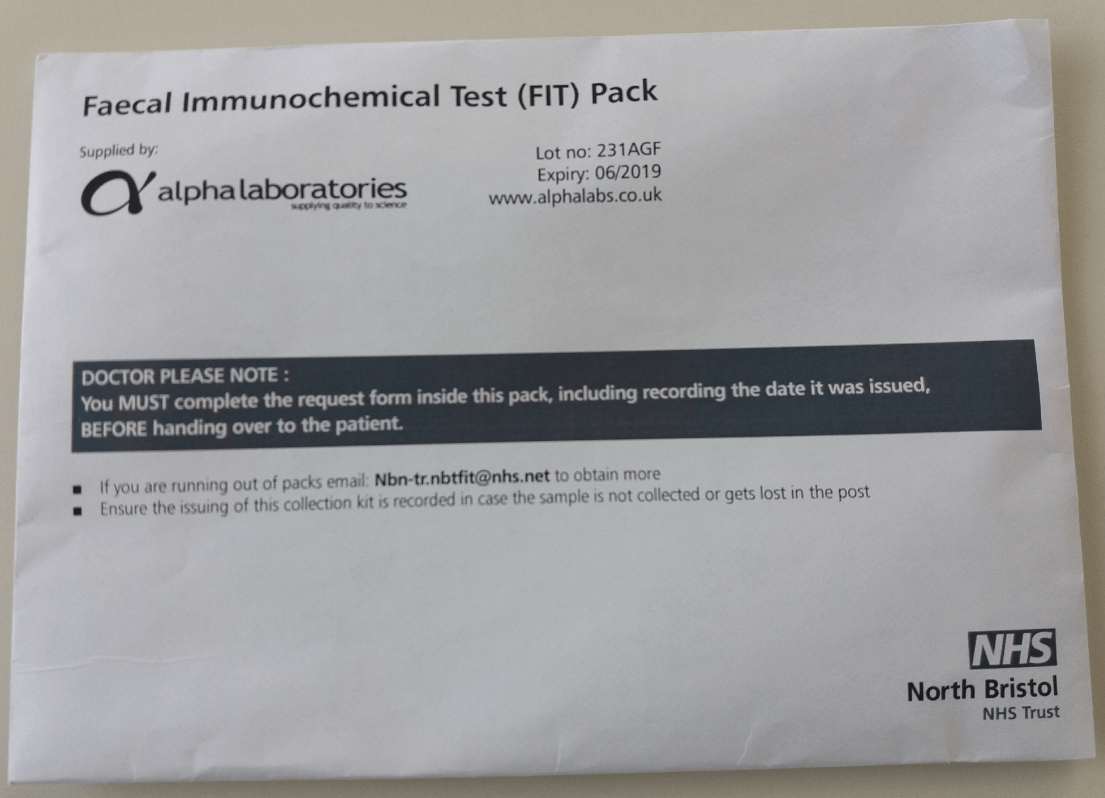
The pack contains the sample collection device, patient instructions, a referral form and return envelopes.
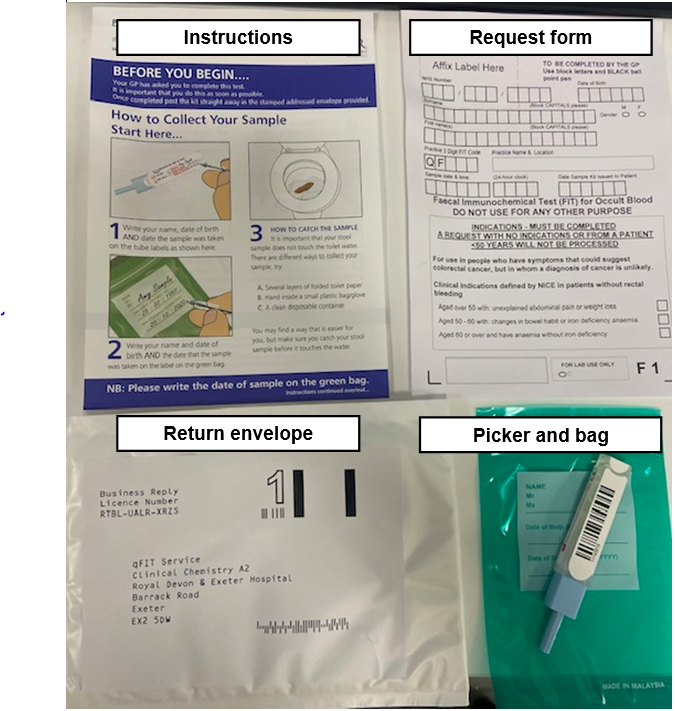
To request a test for eligible patients the referral form (provided inside the pack) will need to be completed and placed back into the pack before handing it to the patient for completion at home. Electronic test requests are not currently available.
GP’s will need to advise patients to return the sample directly to the lab in the pre-paid envelope as quickly as possible. Patients should be advised to follow the collection instructions carefully, including taking care not to let the stool sample touch the water in the toilet bowl.
Because the patient sends off the test themselves, practices may wish to make a note on the patient’s record that a test has been issued and ensure a process is in place to follow up, the result in addition to giving the patient their usual safety netting advice.
Using a READ code will allow you to search for patients who have been advised to send qFIT tests but for whom you have not received a result.
READ Code 4791 (Faecal Occult Blood Requested) is recommended.
SNOMED ID 167666002
GP’s will receive the results of the analysis within 7 working days from the date the test is sent to the laboratory by the patient. If you have not heard the results within 10 days of issuing the test then please contact the patient to ensure the test was sent.
The way results will be communicated will vary according to local arrangements. Practices will be notified individually by the laboratories when the initial supplies of patient packs are distributed.
If the Faecal occult blood test is positive: Consider using a referral for suspected cancer under the local 2WW arrangements. Occult blood in the stool can be caused by a wide variety of benign conditions as well as colorectal cancer, and further assessment may be appropriate to rule out these out before referring.
READ Code 4794 FOB+ve is recommended
Referral forms to secondary care have been updated to allow GP’s to record the FIT test result.
If the Faecal occult blood test is negative: qFIT negative patients have an extremely low risk both of colorectal cancer, and of high risk adenoma. Your patient therefore does not need referral for suspected colorectal cancer, but as always you should consider seeking specialist advice if worrying symptoms persist. In patients with symptoms of significant concern, you should consider non-luminal cancers and may still wish to send a suspected upper GI cancer referral. Advice and guidance services may also be used in line with local arrangements.
The Widlak study (see below) also showed a sensitivity of 86% and Negative Predictive Value of 100% for inflammatory bowel disease.
READ Code 4792 FOB –ve is recommended.
The patient population for whom we are recommending qFIT are at less than 3% risk as they do not meet the NG12 suspected cancer referral criteria. At the test threshold we are using, and in this specific population, research demonstrates a negative predictive value of over 99% and specificity variously reported at 84 or 100%.
It is important to note that in patients with more significant symptoms or other test abnormalities (for example Iron Deficiency Anaemia), the test is less sensitive and may miss some cancers, so it is important to use the test criteria carefully and still refer to NG12 for patients with symptoms of greater concern.
The test may not be suitable for patients who have a disability that would make it difficult for them to complete at home for example those with arthritic hands.
The test instructions are also given in other languages.
Patients, carers and GP’s can feedback their experience of issuing and using the test online. The details of the website will be provided inside the test pack and in supporting documentation provided to GP’s.
Please note this test is not UKAS accredited
Specimen Labelling Procedure